Dry Eye & Cornea
What Causes Dry Eyes?
Dry eyes can develop for many reasons, including:
- Age. Dry eyes are a part of the natural aging process. The majority of people over age 65 experience some symptoms of dry eyes.
- Gender. Women are more likely to develop dry eyes due to hormonal changes caused by pregnancy, the use of oral contraceptives and menopause.
- Medications. Certain medicines, including antihistamines, decongestants, blood pressure medications and antidepressants, can reduce tear production.
- Medical conditions. People with rheumatoid arthritis, diabetes and thyroid problems are more likely to have symptoms of dry eyes. Also, problems with inflammation of the eyelids (blepharitis and meibomian gland dysfunction), inflammation of the surfaces of the eye, or the inward or outward turning of eyelids can cause dry eyes to develop.
- Environmental conditions. Exposure to smoke, wind and dry climates can increase tear evaporation resulting in dry eye symptoms. Failure to blink regularly, such as when staring at a computer screen for long periods of time, can also contribute to drying of the eyes.
- Other factors. Long-term use of contact lenses can be a factor in the development of dry eyes. Refractive eye surgeries such as LASIK, can decrease tear production and contribute to dry eyes.
How Are Dry Eyes Diagnosed?
Dry eyes can be diagnosed during a comprehensive eye exam. Testing, with emphasis on the evaluation of the quantity and quality of tears produced by the eyes, may include:
- Patient history to determine the patient’s symptoms and to note any general health problems, medications or environmental factors that may be contributing to the dry eye problem.
- External examination of the eye, including lid structure and blink dynamics.
- Evaluation of the eyelids and cornea using light and magnification.
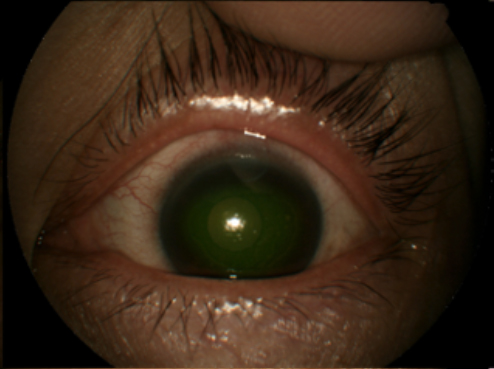
- Measurement of the quantity and quality of tears for any abnormalities. Special dyes may be put in the eyes to better observe tear flow and to highlight any changes to the outer surface of the eye caused by insufficient tears.
With the information obtained from testing, your optometrist can determine if you have dry eyes and advise you on treatment options.
How Are Dry Eyes Treated?
Dry eyes can be a chronic condition, but your optometrist can prescribe treatment to keep your eyes healthy and comfortable and to prevent your vision from being affected.
Preservative Free Artificial Tears
Mild cases of dry eyes can often be managed using over-the-counter preservative-free artificial tears. These can be used as often as needed to supplement natural tear production. Artificial tears that have preservatives can actually make dry eye worse. People with dry eyes that don’t respond to artificial tears alone will need to take additional steps to treat their dry eyes.
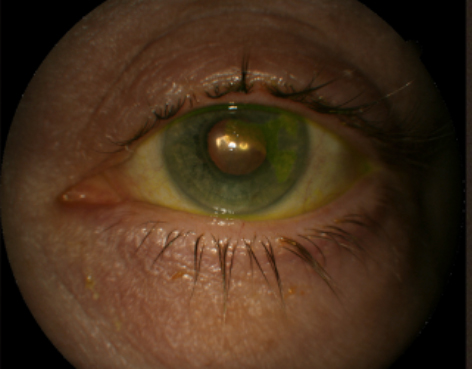
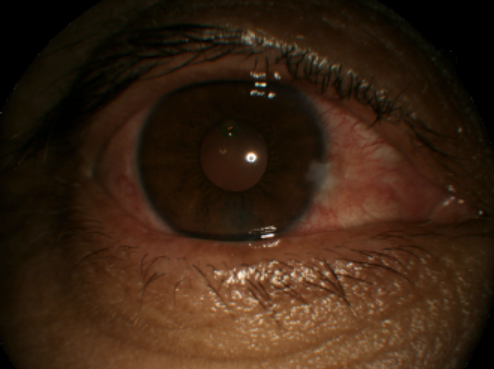
Picture of Meibomian Gland Dysfunction (Above)
Eyelid Scrubs, Hot Compress Masks, Omega-3 Vitamins & TearCare
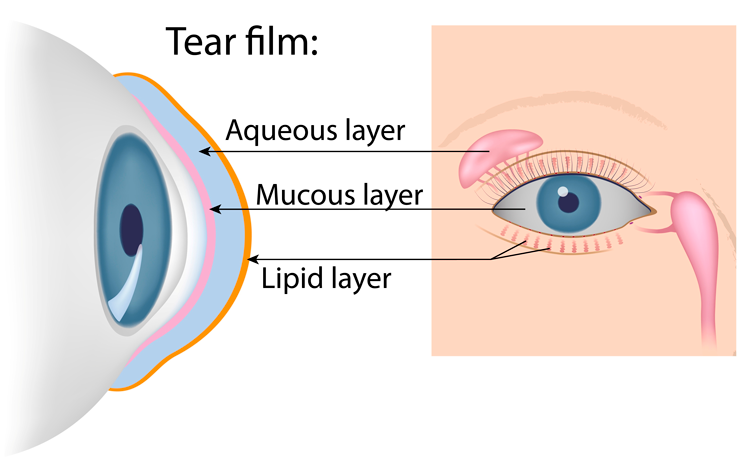
Meibomian glands are on the upper and lower eyelids, when they become clogged, the oils that prevent the tears from evaporating cannot get into the tear film. This is called meibomian gland dysfunction (or blepharitis). Eyelid scrubs, a hot compress mask and omega-3 vitamins can help unclog those glands. Additionally, an in-office device called TearCare® heats the glands for 15 minutes which melts the meibum. Once melted, your doctor will clear those glands with another instrument.
Prescription Eye Drops
Your optometrist can prescribe eye drops (Xiidra and Restasis) that increase tear production and decrease inflammation in the tear film.
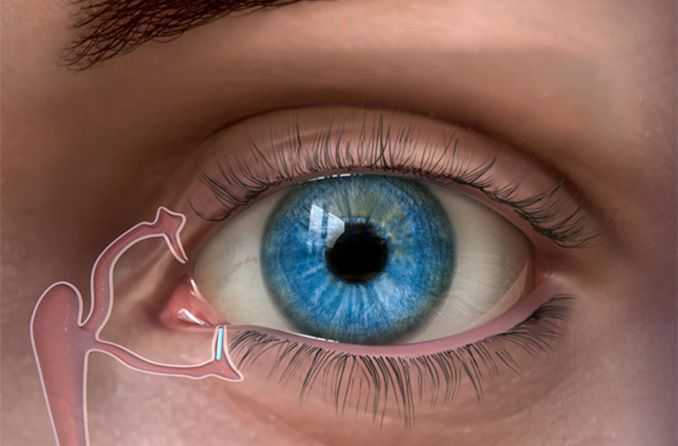
Punctal Plugs
Keeping natural tears in the eyes longer can reduce the symptoms of dry eyes. This can be done by blocking the tear ducts (i.e. punctum) through which the tears normally drain with Punctal Plugs. Punctal Plugs are tiny silicone or gel-like plugs that block the tear ducts. The goal is to keep the available tears in the eye longer to reduce problems related to dry eyes.
Amniotic Membrane Tissue
Amniotic membrane tissue comes from the innermost layer of the placenta. Amniotic membrane tissue contains stem cells that can help decrease inflammation and rehabilitate the ocular surface for select dry eye patients.
Contact Lenses for Dry Eyes
Daily Disposable Soft Contact Lenses
Dry eyes can make wearing contact lenses difficult and cause a number of symptoms, including blurred vision, dryness, grittiness, burning, redness and foreign body sensation. Think of soft contact lens like a sponge. They absorb tears from the tear film and therefore dry the eyes out. Certain soft contact lens materials work better than others for dry eyes. Often, daily disposables contact lenses are best because replacing your contact lenses more frequently reduces dry eye symptoms.
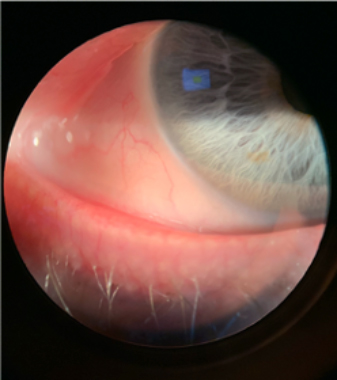
Scleral Contact Lenses
If you’ve been told in the past that you cannot wear contact lenses because of dryness, ask us about scleral contact lenses. Scleral contacts are large-diameter gas permeable contact lenses specially designed to vault over the entire cornea and rest on the eye called the sclera. The space between the cornea and the back surface of a scleral lens acts as a fluid reservoir to provide comfort for people with dry eyes who otherwise could not tolerate wearing contact lens. Unlike soft contact lenses that contribute to dryness, scleral contact lenses are used to treat dry eye by bathing the cornea with a preservative free solution.
Our Dry Eye & Cornea Specialists: Dr. Emily Felouzis, Dr. Sarah Flanagan, Dr. Michelle Moscow, Dr. Scott Moscow, Dr. Ashleigh Sprouse