Retina
What Is the Retina?
The retina is layer at the back of the eyeball containing rods and cones, cells that are sensitive to light. Rods and cones trigger nerve impulses that pass via the optic nerve to the brain. The brain interprets the nerve impulses and forms a visual image.
Retinal Conditions
Artery Occlusion
A retinal artery occlusion occurs when there is a blockage in one of the blood vessels that supplies blood to the eye. This blockage prevents oxygen and important nutrients from reaching the retina, the nerve layer in the back of the eye that senses light. A retinal artery occlusion causes a painless and sudden loss of vision in one eye that can affect all or part of the visual field depending on whether it affects the central artery or a branched artery. It is important to receive treatment immediately or else vision loss in that area can be permanent.
A retinal artery occlusion is diagnosed when your eye care provider examines the inside of your eye by dilating your pupils. Additionally, the doctor may also use a special camera to take a picture of the back of your eye to view the arteries. To dislodge or break up the blockage your eye care professional may decrease the pressure in the eye or massage your eye. Depending on the artery and how soon the blockage is treated you may be able to regain your vision. Because a retinal artery occlusion commonly occurs in people with heart and vascular diseases you may be evaluated and treated for these conditions to prevent future medical emergencies such as a stroke.
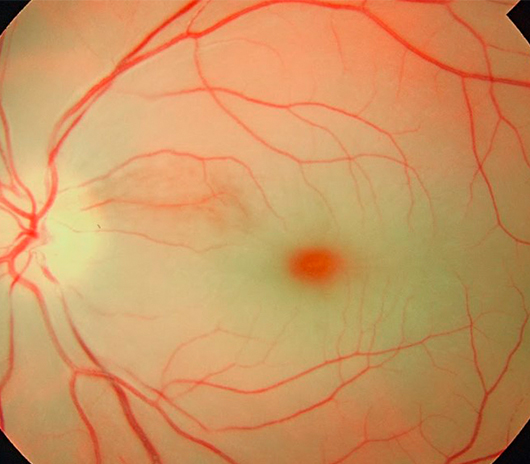
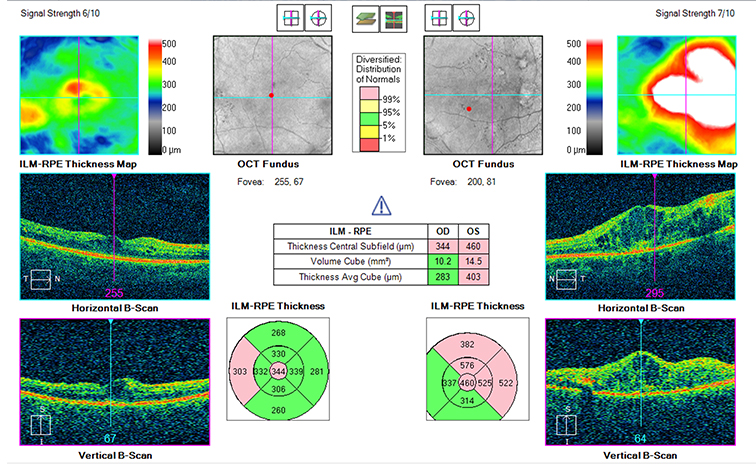
Central Serous Retinopathy
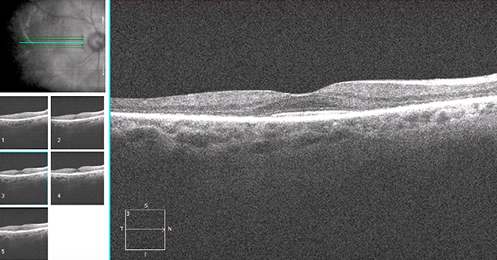
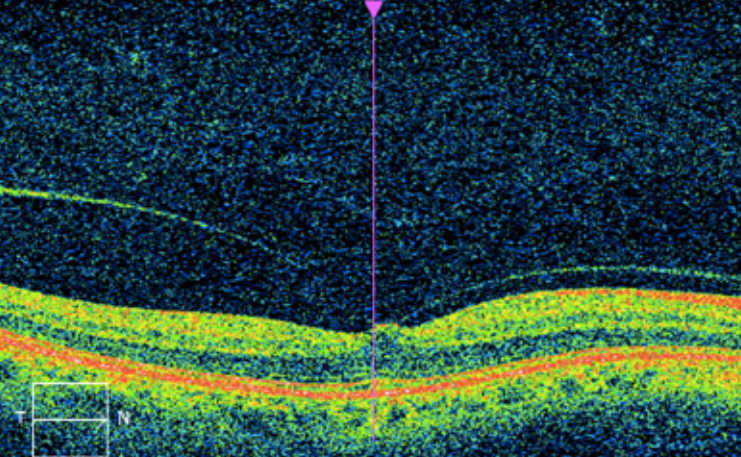
Central Serous Retinopathy (CSR) occurs when fluid builds up under your retina. This buildup of fluid causes blurred or distorted vision. The causes of CSR are not entirely understood, but high levels of corticosteroid, a hormone, can cause worsening of the condition. Stress, pregnancy, high blood pressure and certain medications are known to cause increased levels of corticosteroid.
To determine if you have CSR, your eye care professional will perform an OCT, a non-invasive scan of the retina that allows them to see a cross-sectional view of the retina. Another test, called fluorescein angiography will take pictures of the blood flow through the retina to look for sources of fluid leakage.
Fluid buildup usually resolves after 3 to 6 months, but if it persists or returns after resolution, more in-depth treatments should be performed. More in-depth treatments include laser treatment, photodynamic therapy, intravitreal injections, or oral medications. It is important to use an Amsler grid at home to monitor for any changes and continue all regular visits with your eye care professional.
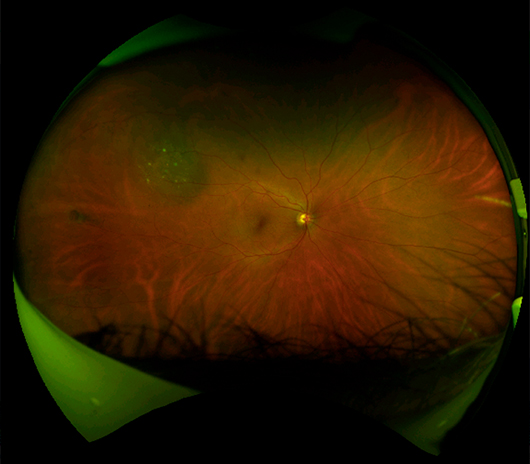
Choroidal Nevus
A choroidal nevus is a flat, benign, pigmented area that appears in the back of the eye. A choroidal nevus represents an accumulation of pigment cells in the choroid. There are usually no symptoms associated with choroidal nevi. A choroidal nevus can only be seen by an eye care specialist. Similar to a nevus on the skin, a choroidal nevus has the potential to become a malignant melanoma. It is important for your optometrist to observe the nevus for change every 6-12 months.
Congenital Hypertrophy of the Retinal Pigment Epithelium (CHRPE)
Congenital Hypertrophy of the Retinal Pigment Epithelium (CHRPE) occurs when the pigmented layer of the retina, the RPE, is thicker than normal. Typically, there are no symptoms associated with a CHRPE. A CHRPE has the tendency to enlarge over time but is not malignant. A CHRPE is diagnosed by an eye specialist looking at the retina.
Cystoid Macular Edema
Macular edema is a condition that occurs when fluid builds up within the macula, the central area of the retina responsible for sharp vision. The buildup of fluid causes the macula to swell, disrupting its normal shape and resulting in damage to vision. The two main causes of cystoid macular edema are inflammation and vitreous traction.
Symptoms associated with macular edema include blurred vision, distortion of images, missing areas of vision or a change of contrast in vision. If macular edema is left untreated, the swelling can cause these vision problems to progressively worsen. If any of these vision problems occur its important to see an eye care professional immediately.
Floaters
Floaters are small, semi-transparent or cloudy particles within the vitreous, which is the clear, jelly-like fluid that fills the inside of your eyes. These spots can appear as specks of various shapes and sizes, threadlike strands or cobwebs. Because they are in your eyes, they move as your eyes move and seem to dart away when you try to look at them directly.
Spots are often caused by small flecks of protein or other matter that became trapped when your eyes formed before birth. They can also appear as the vitreous fluid deteriorates due to aging. Also, certain eye diseases or injuries can cause the appearance of spots.
Most spots are harmless, and they rarely limit vision. However, spots can be an indication of a more serious problem. See your doctor of optometry for a comprehensive examination if you suddenly start seeing more spots, especially in your central vision.
Your doctor of optometry can determine if what you are seeing is harmless or a symptom of a more serious problem that requires treatment.
Hypertensive Retinopathy
Systemic hypertension (high blood pressure) not only affects the heart and kidneys but it also affects the eye and can cause serious vision problems if left untreated. Increased blood pressure causes the walls of the blood vessels to thicken which reduces the amount of space in the blood vessels. This reduction of space in the blood vessels makes it harder for blood to reach the retina in the back of the eye, this is called hypertensive retinopathy. Late stage symptoms include decreased eyesight, double vision, or blind spots accompanied by headaches.
In order to diagnose hypertensive retinopathy, the retina is evaluated with a dilated eye exam. During this exam the doctor is looking for narrowed blood vessels or signs of leakage. Treatment of hypertensive retinopathy includes controlling high blood pressure through lifestyle changes, medication, and careful monitoring.
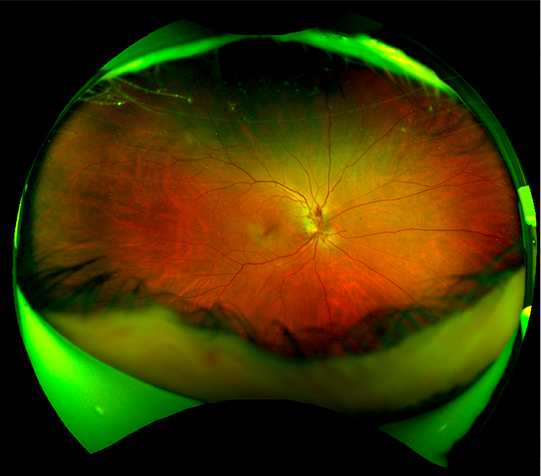
Lattice Degeneration
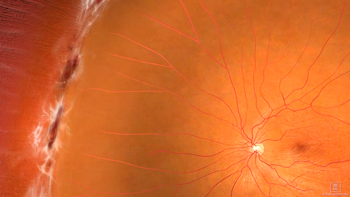
Lattice degeneration is a condition that consists of abnormal thinning of the peripheral retina. With lattice degeneration, the retina is more vulnerable to developing tears, breaks, or holes that could eventually lead to a retinal detachment. If you have been diagnosed with lattice degeneration it is important to be closely monitored. Lattice degeneration does not have any associated symptoms and the only way to diagnose this condition is by having an eyecare professional look at the back of the eye. If lattice results in a retinal tear or detachment you should be aware of symptoms that include blurred vision, flashing lights, floaters, or a veil of black over your visual field. Treatment for lattice includes regular monitoring and sometimes preventative laser therapy or cryotherapy is recommended.
Macular Degeneration
Age-Related Macular Degeneration (AMD) is the leading cause of severe vision loss in adults over age 50. The Centers for Disease Control and Prevention estimate that 1.8 million people have AMD and another 7.3 million are at substantial risk for vision loss from AMD.
Caucasians are at higher risk for developing AMD than other races. Women also develop AMD at an earlier age than men.
This eye disease occurs when there are changes to the macula, a small portion of the retina that is located on the inside back layer of the eye. AMD is a loss of central vision that can occur in two forms: “dry” (atrophic) and “wet” (exudative).
Most people with macular degeneration have the dry form. While there is no specific treatment for dry AMD, studies have shown a potential benefit from vitamin supplements a Mediterranean diet and cessation of smoking. The less common wet form may respond to intraocular injections of anti-VEGF medications if detected and treated early.
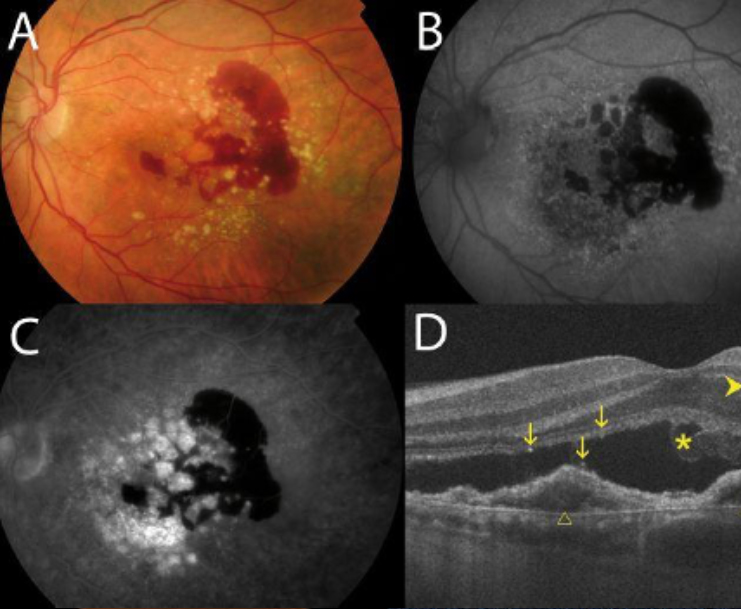
Age-Related Macular Degeneration (AMD) Wet (i.e. Exudative Macular Degeneration)
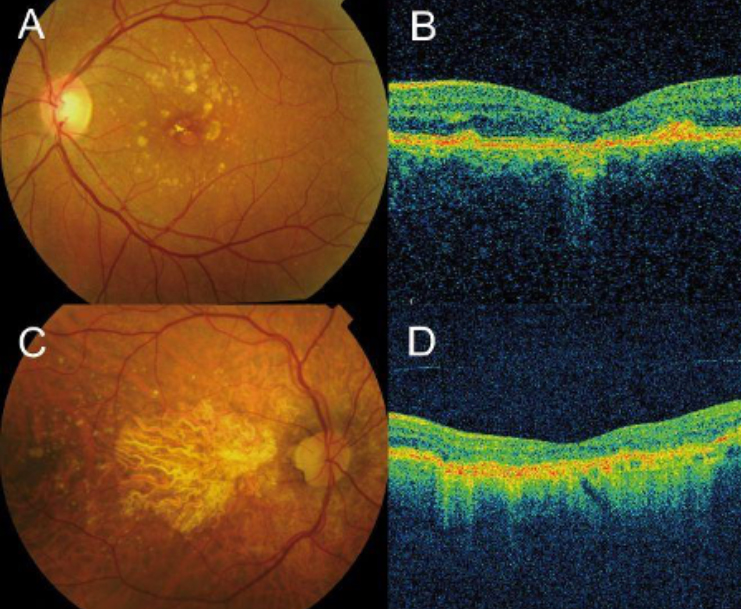
Atrophic Macular Degeneration (a severe form of Dry AMD)
Symptoms and Diagnosis of AMD
In its early stages, the following signs of macular degeneration can go unnoticed.
- Gradual loss of ability to see objects clearly.
- Shape of objects appears distorted.
- Straight lines look wavy or crooked.
- Loss of clear color vision.
- A dark or empty area in the center of vision.
If you experience any of the above signs or symptoms, contact your doctor of optometry immediately for a comprehensive eye examination. Your optometrist will perform a variety of tests to determine if you have macular degeneration or any other eye health problems.
Central vision that is lost to macular degeneration cannot be restored. However, low-vision devices, such as telescopic and microscopic lenses, can maximize existing vision.
Treatment of AMD
With “dry” macular degeneration, the tissue of the macula gradually becomes thin and stops working properly. There is no cure for dry AMD, and any loss in central vision cannot be restored.
However, researchers and doctors believe there is a link between nutrition and the progression of dry AMD. Making dietary changes and taking nutritional supplements can slow vision loss.
Less common, “wet” macular degeneration occurs when fluids leak from newly formed blood vessels under the macula. This leakage blurs central vision. Vision loss can be rapid and severe.
If detected early, wet AMD can be treated with intraocular injections of anti-VEGF medications.
Researchers have linked eye-friendly nutrients such as lutein and zeaxanthin, vitamin C, vitamin E and zinc to reducing the risk of certain eye diseases, including macular degeneration. For more information on the importance of good nutrition and eye health, please see the diet and nutrition section.
Macular Holes
The macula is the portion of the retina responsible for detailed central vision. As we age the vitreous inside the eye can shrink and pull on the retina, creating a hole in the macula. In early stages, a macular hole can cause a slight distortion or blurriness in the central vision. Reading and performing other routine tasks such as driving, may become difficult. If the condition progresses, patients will experience a loss of central vision. If left untreated, the vision loss from the macular hole can be permanent. Treatment for a macular hole is a vitrectomy.
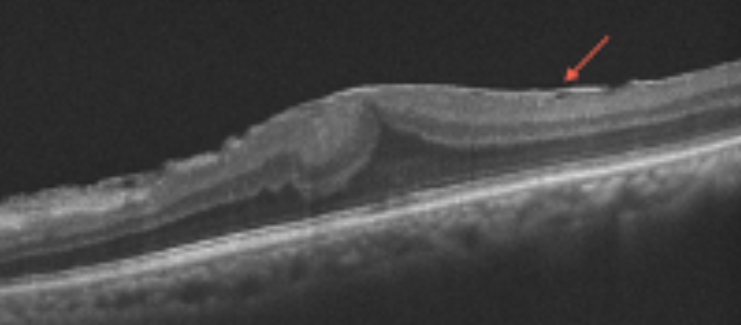
Macular Pucker/Epiretinal Membrane
As we age the vitreous inside the eye can shrink and pull on the macula. When this occurs in the macular area, the retina initiates a healing response with a migration of cells found within the retina. These cells form a thin layer of scar tissue known as a macular pucker or epiretinal membrane.
Symptoms include blurred or distorted vision. This condition requires routine visits with your eye care professional.
Ocular Histoplasmosis
Ocular histoplasmosis is caused by Histoplasma capsulatum, a fungus commonly found in the soil of the central and eastern United States. Ocular histoplasmosis occurs as a secondary infection when a retinal scar allows the formation of abnormal blood vessels under the retina. As these blood vessels grow, they ooze clear fluid and blood which can affect vision.
Ocular histoplasmosis is treated with laser surgery, photodynamic therapy, or injections of medications to make the abnormal blood vessels stop leaking.
Ocular Migraine
An ocular migraine is caused when the blood vessels in the part of the brain responsible for vision temporarily spasm which can be due to reduced blood flow. Ocular migraines cause a disturbance in vision, known as an aura. An aura typically lasts from several minutes to about an hour. An aura may appear as a blank spot, flickering colored lights, zig zag lines or a blurred area of vision like looking through heat waves.
After episode of visual distorting the person may feel completely back to normal; if this is the case then no treatment is needed even if the person experiences multiple episodes in a short period of time. Others may experience an altered sense of awareness after an episode; lights and sounds may be unusually intense; they may feel nauseous or have a headache. If a person experiences these other symptoms, then their ocular migraine may be progressing into a classic migraine and they should be referred to their medical doctor for treatment.
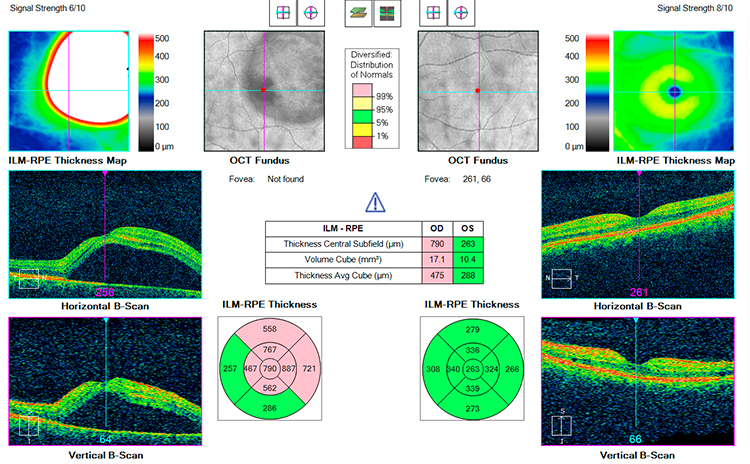
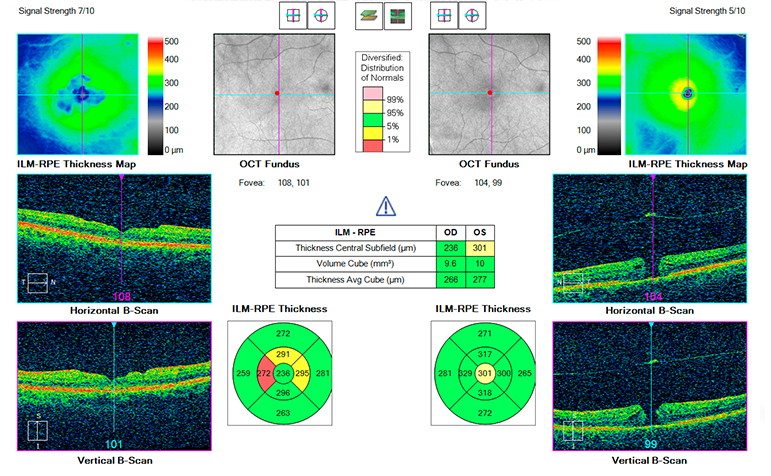
Plaquenil Toxicity
Plaquenil (hydroxychloroquine) is a medication prescribed for inflammatory diseases such as rheumatoid arthritis or lupus. If you take plaquenil, it is important to be aware on how it can affect your vision. Plaquenil can result in the build up of deposits in the cornea, which usually does not affect your vision. Most important, although uncommon, plaquenil can also cause retinal toxicity resulting in irreversible vision loss. This can progress even after stopping plaquenil. Due to this risk of irreversible vision loss it is extremely important to have your vision tested before or as soon as you start this medication. The risk of retinal toxicity increase over time, so you should receive annual retinal toxicity screenings after 5 years of Plaquenil use.
Risk factors include long term use of medication, high dose of medication relative to body weight, previous retinal conditions, or kidney or liver disease. If you are high risk, then you may need to be screened more frequently.
Testing for toxicity includes a retinal exam, visual field test, and an OCT scan of the macula. Early screening is essential in order to monitor changes and minimize loss of vision.
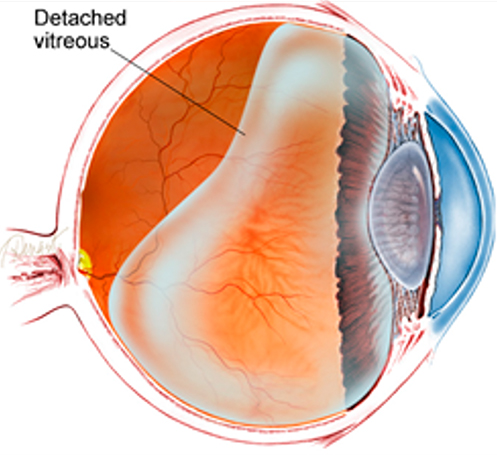
Posterior Vitreous Detachment
As we age the vitreous inside the eye can shrink and may eventually separate from the inside surface of the eye, this is called a posterior vitreous detachment (PVD). When the vitreous pulls free from the eye, it is often accompanied by flashes of light and the appearance of tiny black spots in the vision. Generally, PVDs are not dangerous but in certain cases they can lead to more serious conditions. If left untreated, these conditions can lead to vision loss and sometimes blindness. It is recommended that anyone with symptoms of a posterior vitreous detachment should have an eye exam immediately to make sure that a more serious problem is not present.
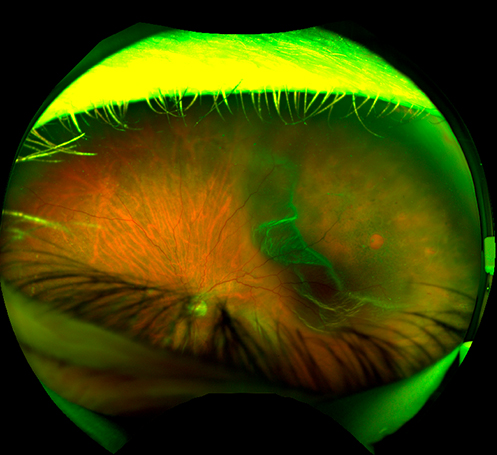
Retinal Detachment
A retinal detachment occurs when the retina’s layers separate. Any portion of the retina that is detached cannot send visual signals to the brain. If left untreated, a retinal detachment can cause devastating damage to an individual’s vision. Symptoms of a retinal detachment include flashes, floaters, or a veil of black over one’s vision. Retinal detachment is considered an ocular emergency that requires immediate medical attention.
Retinopathy of Prematurity
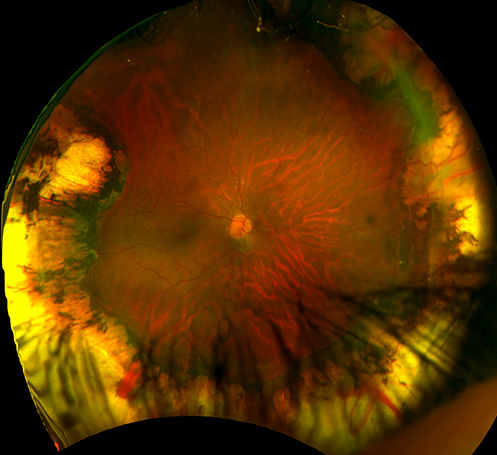
Retinopathy of Prematurity (ROP) is a condition of the blood vessels of the eye that usually occurs in premature infants. The blood vessels in the retina are formed during pregnancy. When babies are born prematurely, these vessels may not be fully formed. In order to compensate, the retina triggers disorganized growth of blood vessels. Without treatment, the blood vessels can pull on the retina and damage the retina with scar tissue or cause the retina to detach, leading to a vision loss. Retinopathy of Prematurity also increases the risk of nearsightedness (myopia), eye muscle misalignment, glaucoma, and cataracts.
When testing for Retinopathy of Prematurity the doctor will use eye drops to dilate the baby’s pupils and examine the back of the eye and determine the stage of the condition. Classifying the stage of the condition helps determine the best course of treatment. If Retinopathy of Prematurity requires treatment, the most common treatment is laser therapy or cryotherapy. Early detection, regular follow-up appointments throughout infancy and early childhood, and proper treatment can improve your baby’s chances to have normal vision.
Tumors of the Eye
The most common type of tumor of the eye in adults is melanoma. Primary melanoma of the eye is rare. Risk factors include excessive exposure to sunlight, fair-skin, and light color eyes. Most tumors of the eye initially have no symptoms associated but you may become symptomatic as the tumor enlarges.
Melanoma can be detected by routine eye exams that include dilation of the eye to observe the posterior part of the eye. Small/early melanomas can be treated by lasers, brachytherapy, or radiation but enucleation (removal of the eye) may be necessary in some cases. The prognosis depends on the size and cell type.
Uveitis
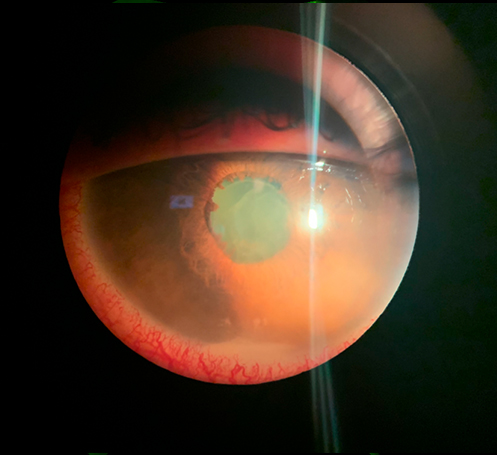
Uveitis is inflammation of the uvea, which is the middle layer of the eye’s surface, comprised of the iris, choroid, and ciliary body. Uveitis can be caused by a variety of factors including bacterial infections, viral infections, an eye injury or an autoimmune disorder.
Common symptoms of uveitis include light sensitivity, redness of the eye, and floaters. Uveitis is often chronic and can be serious, so proper care and early treatment is critical. An eye care professional will test the vision and examine the eye to detect signs of inflammation.
If left untreated it can even cause vision loss. Treatment for uveitis includes wearing dark sunglasses and medication to dilate the pupil which allows the iris to rest and heal. Additionally, steroids are prescribed to decrease inflammation. Proper treatment and follow up care are critical for a healthy recovery.
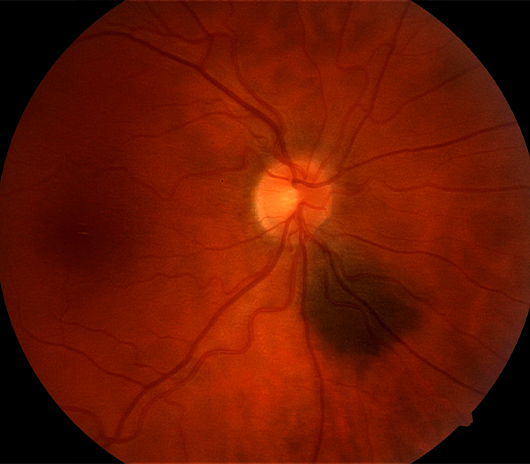
Vein Occlusion
Like every other tissue in the body, the retina is nourished by a system of blood vessels. The retinal arteries and veins originate at the optic nerve and spread across the entire retina. If a clot or obstruction to blood flow occurs in a retinal vein it can affect the entire retina if it occurs at the central vein where the optic nerve is, this is a central retinal vein occlusion. If it occurs further out from the center it only affects a portion of the retina, this is a branch retinal vein occlusion.
Vein occlusions cause fluid or blood to build up in the affected parts of the retina, including the part of the retina that provides sharp vision called the macula. Symptoms include sudden or severe blurring or dimming of vision. Overtime these acute symptoms may turn into permanent vision loss. Retinal vein occlusion requires prompt attention by an eye doctor because in many cases treatment can be provided to reduce swelling of the macula and reduce other complications. Patients with hypertension, diabetes, and atherosclerosis are more at risk for developing vein occlusions.
Vitreo-Macular Traction (VMT)
The vitreous is a clear, jelly-like fluid that fills the inner portion of the eye. With time, the vitreous deteriorates as it becomes more like water and less like jelly. As that happens, the vitreous should separate from the retina. VMT occurs when vitreous gets stuck on the retina starts pulling the retina. VMT is a vision-threatening condition that can lead to a macular hole or retinal detachment.
Our Retina Specialists: Dr. Emily Felouzis, Dr. Sarah Flanagan, Dr. Michelle Moscow, Dr. Scott Moscow, Dr. Ashleigh Sprouse